Two tiny groups of brain cells, right next to each other, play a key role in driving feeding — and stopping. The brain’s own opioid system also gets involved.
1:42 PM
Author |
Almost everyone knows the feeling. You're at a restaurant or a holiday meal, and your stomach is telling you it's full, so logically you know you should stop eating.
But what you're eating tastes so good, or your friends and family are still eating, or you don't get this treat very often. So you keep going.
A new study in animals explores the mystery of why this happens, at the most basic level in the brain. It shows that two tiny clusters of cells battle for control of feeding behavior — and the one that drives eating overpowers the one that says to stop.
It also shows that the brain's own natural opioid system gets involved — and that blocking it with the drug naloxone stopped over-eating.
The researchers studied mice, not over-eating humans. But they do note that the findings could help inform the fight against the global obesity epidemic.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
The team, from the University of Michigan Molecular and Behavioral Neuroscience Institute, published their work in the Proceedings of the National Academy of Science.
The two groups of brain cells they looked at, called POMC and AgRP, are next-door neighbors in a deep brain region called the arcuate nucleus, or Arc, within a larger region called the hypothalamus, which is a master regulator of motivated behaviors.
Neuroscientist and U-M Department of Psychiatry professor Huda Akil, Ph.D., led the Michigan Medicine research team. She says the discovery involved a strong dose of serendipity.
"We used a transgenic approach to specifically address the POMC neurons for optogenetic stimulation, and we expected to see a decrease in appetite. Instead, we saw a really remarkable effect," she says. "The animals ate like crazy; during the half hour after stimulation, they ate a full day's supply of food."
A tale of two genes
Previous research, including work done in several U-M laboratories, showed that the Arc region, and specifically POMC and AgRP neurons, play key roles in feeding behavior.
The gene called POMC (short for pro-opiomelanocortin) has multiple functions: it encodes a stress hormone called ACTH, a natural opioid called beta-endoprhin, and several other molecules called melanocortins.
The first mammalian gene to be cloned, it was also the first gene that scientists visualized in the brain of a mammal using a technique called in situ hybridization — work that was led by U-M psychiatry researcher Stan Watson, M.D., Ph.D., who also co-authored the new paper. Another U-M researcher, Roger Cone, Ph.D., first cloned the receptors for POMC-produced melanocortins, and demonstrated their role in food intake, energy regulation and obesity. Cone directs the U-M Life Sciences Institute.
POMC's products get opposition from products of the AgRP gene, whose name is short for Agouti-Gene-Related Peptide. Watson also mapped the location of AgRP cells in the brain, and Cone's team determined their role in feeding and obesity.
MORE FROM MICHIGAN: Subscribe to our weekly newsletter
In general, POMC acts like a brake on feeding when it gets certain signals from the body, and AgRP acts like an accelerator pedal, especially when food is scarce or it's been some time since a meal.
But the new study shows for the first time how their activity relates to one another, thanks to a technique called optogenetics. Focusing on unique molecular features of a particular group of neurons,makes it possible for scientists to target, or address, those cells specifically and activate them selectively. The work was funded by the National Institutes of Health, the Hope for Depression Research Foundation and the Pritzker Neuropsychiatric Research Consortium
A hunt for answers
The serendipitous optogenetic finding about the over-eating mice set off a search for the reason why they overate, led by Michigan Medicine research scientist Qiang Wei, Ph.D., working with others in Akil's lab and with Raju Tomer of Columbia University and Karl Deisseroth of Stanford University.
The answer was that while they were optogenetically stimulating the POMC cells, they were also unintentionally stimulating a subset of AgRP cells nearby. The two types of cells originate from the same parent cells during embryonic development. That common heritage meant that the transgenic approach Akil and her colleagues used to address POMC captured not only the POMC neurons but also a segment of the AgRP neuronal system.
In other words, they had turned on both the brake and the gas pedal for eating. When both types of cell got activated, the "keep eating" signal from AgRP cells overpowered the "stop eating" signal from POMC cells. "When both are stimulated at once, AgRP steals the show," says Akil.
Then the researchers used a different technique, addressing the cells with an injected virus rather than a transgene, to focus the optogenetic stimulation on just POMC neurons and ensure that AgRP neurons didn't get activated.
They found that stimulating just POMC cells caused a significant decrease in eating – and were surprised at how rapidly it happened. Akil notes that past research had shown slow effects of POMC stimulation on eating — but in these previous experiments, mice had recently eaten, while the mice in the U-M study were slightly hungry.
READ MORE: Brain Protein That Helps Regulate Body Fat May Guide Anti-Obesity Drugs
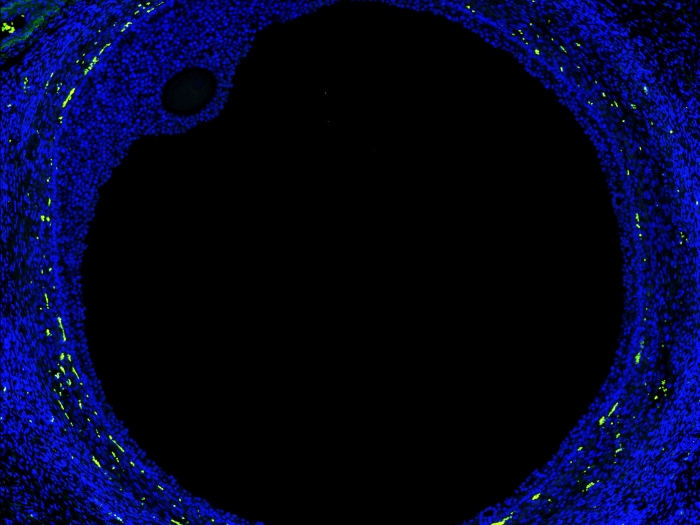
The team also used a new method called CLARITY to visualize in 3-D the pathways that start from POMC and AgRP neurons. These pathways of neurons, once activated, can trigger either a sense of feeling full – called satiety -- or the drive to eat. They stitched together images of activated neurons in a computer, to create 3-D videos that show the neurons' reach. The videos can be seen here: http://michmed.org/EXGOq
Then, the researchers used a method called c-fos activation to dig deeper into the downstream effects of POMC and AgRP neuron activation – and showed that its effects spread throughout the brain, including in the cortex, which governs function like attention, perception, and memory.
Since POMC encodes a natural opioid (B-Endorphin), the authors asked whether activation of this system triggers the body's own natural painkiller system, called the endogenous opioid system. They found that activation of POMC blocked pain, but that this was reversed by the opioid antagonist drug naloxone.
Interestingly, the activation of AgRP, which triggered feeding, also turned on the opioid system in the brain. "When we administered naloxone, which blocks opioid receptors, the feeding behavior stopped," says Akil. "This suggests that the brain's own endogenous opioid system may play a role in wanting to eat beyond what is needed."
The research was funded by the National Institutes of Health, the Hope for Depression Research Foundation, and the Pritzker Neuropsychiatric Research Consortium.
More than just metabolic signals
The involvement of the cortex and opioid systems lead Akil and her colleagues to think about how the results might relate to the human experience. Though mice and humans are very different, Akil speculates that the bombardment of our senses with sights and smells related to food, and the social interactions related to food, may be involved in encouraging overeating.
Perhaps, she says, these factors combine to trigger us to become interested in eating when we're not even hungry, causing the "stop" signal to lose out to the "keep going" signal.
"Our work shows that the signals of satiety — of having had enough food — are not powerful enough to work against the strong drive to eat, which has strong evolutionary value," she says. She notes that other researchers are looking at opiate receptor blockers as potential diet aids, and that it's also important to study the pathways that are activated by the products of both POMC and AgRP cells, as well as individual differences in all these systems.
Many studies in humans have looked at the metabolic aspects of the drive to eat, and overeat — for instance, the metabolic signals that travel between the body and brain in the form of peptides such as leptin and ghrelin. But Akil says there appears to be a strong neural system involved in overeating that results from perceptual, emotional and social triggers, and that is not receiving sufficient scientific attention.
"There's a whole industry built on enticing you to eat, whether you need it or not, through visual cues, packaging, smells, emotional associations," she says. "People get hungry just looking at them, and we need to study the neural signals involved in those attentional, perceptional mechanisms that drive us to eat."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!