Reactivating genes normally active before birth could prevent the harmful effects of a blood disorder with few treatment options.
7:00 AM
Author |

It is the most common inherited blood disorder in the U.S., affecting 70,000 to 100,000 Americans. Yet there is only one effective treatment — hydroxyurea — which inexplicably works in only about half of patients.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, Google Play and Stitcher.
Sickle cell disease is the result of a genetic mutation that affects red blood cells' ability to deliver oxygen. Remarkably, the millions of people worldwide who carry just one copy of the mutated gene are protected against severe malaria. In fact, the sickle gene tends to cluster in geographic regions that are endemic for malaria or were in the past, including Africa, Central and South America, the Middle East and the Mediterranean.
SEE ALSO: Most Children with Sickle Cell Anemia Not Receiving Key Medication
People who inherit two copies of the gene, however, can develop debilitating symptoms — or worse.
"Only about 50 percent of children born with sickle cell survive to 5 years of age. Even in adults, it's a lethal, devastating disorder," says Doug Engel, Ph.D., professor of cell and developmental biology at the University of Michigan Medical School. He and his colleagues have been interested in the genes that regulate the production of globins, the proteins that bind to and carry oxygen, for nearly 45 years. But only in the past 10 to 15 years have advances in genetics offered some hope for developing new treatments.
Back to the womb
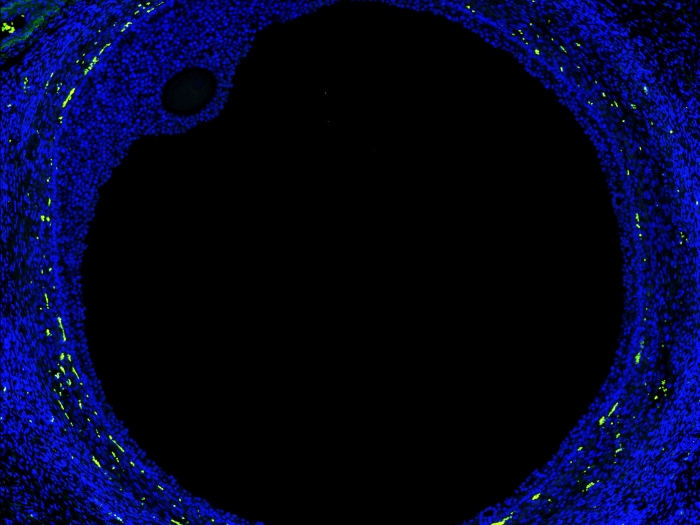
Interestingly, babies born with two copies of the mutated gene don't develop signs of the disease until around 6 months of age. Before birth, fetuses have a different form of the hemoglobin protein, called fetal hemoglobin, which can bind to more oxygen from the mother's blood. Shortly after birth, synthesis of this fetal globin gene begins to switch to the adult beta globin form. People with two copies of the mutated beta globin gene produce an abnormal hemoglobin that aggregates to form long, twisted strands, causing red blood cells to become stiff and stretched into a telltale crescent moon or sickle shape.
Only about 50 percent of children born with sickle cell survive to 5 years of age. Even in adults, it's a lethal, devastating disorder.Doug Engel, Ph.D.
SEE ALSO: Finding Curative Potential Within a Gene Mutation
"These red blood cells are easily broken, which causes inflammation and anemia," Engel says. These sickled cells can get caught inside small blood vessels, causing pain and organ damage.
Engel's group is trying to better understand the mechanisms behind the switch from fetal gamma globin to adult beta globin, with the aim of potentially forcing a switch back to alleviate the signs and symptoms of sickle cell disease.
Reverse engineering
In 2002, Engel's group discovered a complex that represses the expression of the fetal globin gene. Nicknamed DRED (direct repeat erythroid-definitive), the complex is comprised of at least a dozen proteins, including several that haven't been identified yet. The ones that have been identified work by repressing chromatin, Engel says. Chromatin is a mass of DNA and proteins that organizes chromosomes inside cells. If chromatin is repressed, it cannot be transcribed, blocking expression of those genes.
The team's goal then has been to identify the players within the DRED complex to, in a sense, block the blockers and reactivate fetal hemoglobin. "One of the enzymes we focused on, called LSD1, we showed that by inactivating it, we could pretty dramatically increase the levels of fetal hemoglobin," Engel says.
The new work, co-led by Engel lab member Lei Yu, Ph.D., and Natee Jearawiriyapaisarn, Ph.D., of Mahidol University in Thailand, details a new DRED co-repressor, called BAP1, and a protein that forms the scaffold of the DRED complex itself, called NCoR1.
MORE FROM MICHIGAN: Sign up for our weekly newsletter
"Each of the proteins in the complex has a distinct function, but they vary in what level of action they are taking," Engel says. "The co-repressors are the enzymes that control chromatin dynamics, and NCoR1 is the link between those enzymes and the DNA-binding proteins."
The work is published in the latest issue of Genes & Development.
Engel explains that the data so far show that inactivating BAP1 maybe be equally as good as inactivating LSD1 for reactivation of the fetal globin genes. "There's reason to believe that inactivation of a couple of these enzymes with very low drug doses may be more beneficial than targeting any one of them alone," he notes. "The possibility of developing a combinatorial therapy that won't have significant side effects is much higher than coming up with a single therapeutic that's going to be the magic bullet."

Explore a variety of healthcare news & stories by visiting the Health Lab home page for more articles.

Department of Communication at Michigan Medicine
Want top health & research news weekly? Sign up for Health Lab’s newsletters today!